Our quick action and the actions of the doctors on duty that day, saved our daughters life and we are forever grateful.
This is Holly’s story.
Wednesday, 6th June 2012 started as any other day. Rushing around getting ready for work, getting our toddler Holly up, fed and dressed to go to daycare. Graeme had already left for work much earlier and our eldest daughter Hannah had gone off to catch the bus to high school. Little did we know that today was a day that will live in our hearts and minds for the rest of our lives and bring about a tremendous realisation of how blessed and lucky we are to have our little girl with us today.
Every anniversary since this day still continues to bring up incredible emotion and we give thanks.
I dropped Holly off at daycare, which was right next door to me at work. She gave me a big kiss and a hug then ran off to play as she would do normally. After going out the door, I would always peek through the window of the door to watch her play with her friends for a couple of minutes, just to make sure that she wasn’t going to cry when I left, but she never cried, she loved being at daycare. However, that morning I was running late and so I didn’t linger to watch her through the window, I didn’t take that time that I always made the effort in doing.
Graeme usually picked Holly up in the afternoons and when he got there at 3:30pm she did as she normally did, ran up to him, he picked her up and gave her a big kiss and cuddle and they went home. In the car on the way home (which was only 5 minutes up the road) she would normally bop away to the radio playing and insist on Graeme turning the music up loud. On this day, she sat there quietly and didn’t seem too interested in chatting or listening to the music. When they got home he asked her if she wanted something to eat and she said no, which was extremely unusual as Holly has always been the best eating baby / toddler I have ever known and always had a huge appetite upon getting home.
Graeme then noticed that she went and lay down on the couch so he put telly on for her to watch while she laid there. After about 15 minutes she then started to cry and when he went to comfort her she started vomiting. He did all the right things, kept giving her fluids and just let her rest on the couch. He rang and left me a message at work at 5:15pm and said that Holly was vomiting and asked what else he should do. I rang him back at 5:30pm and we chatted and I said that I had seen that two of the rooms at daycare had notices on the doors saying they had had cases of gastro in those rooms (but not Holly’s room), so I said that she had probably picked up gastro, so just keep giving her fluids as there wasn’t a lot we could do for that but keep her hydrated.
When I got home and saw Holly she was flopped over the pillow on the couch and her little body was just like a rag doll. I immediately got the thermometer to check her temperature and it came back as 37.8, nothing to really get worried about. I kept checking her temperature, and also checked her body for any rash – thinking more along the lines of chicken pox as Hannah had had chicken pox as a toddler. No rash, nothing to feel alarmed about and so I just kept giving her drinks through a straw but she kept vomiting after each drink. I gave her some Panadol and she slept.
That night I slept out on the couch with her as she cried when I tried to move her. All through the night she continued to vomit and I just kept the bowl handy so that she didn’t have to get up.
Around 6am Holly sat up and just started crying and holding her hand against her forehead, so I knew she was in pain. I got up and moved in front of her and was calling her name and asking her to show me where it hurt. At that point she was staring at me but was not focusing on me. I then said “Holly look at mummy, where’s mummy” and she just wasn’t seeing me. Then her eyes just rolled back and she just started screaming and it was in that instance I felt an urgency I had never felt before. I knew that this was not good, it was not normal and all my instincts were telling me to get her to a hospital quick.
I yelled out to Graeme in the bedroom and when he came out I told him what happened and I said that we needed to get Holly to hospital. I checked her temperature again and it was elevated to 39.2 so I gave her some more panadol, which I thought would also help with the pain in her head. By then Holly was quieter but was just limp and listless and non-responsive.
Graeme said that she was probably really dehydrated and so would be a bit delirious and we should just keep an eye on her and see how she went over the next couple of hours and take her to the doctor when they opened later on around 9am.
I just knew that we had to go, there was just this strong feeling in my gut that things were not right and I felt a little panicked so said to him “no we need to get her to PMH now!!”
He was a little quiet then said “okay but we will go to Joondalup Emergency as traffic will be building up and trying to get into PMH and find parking will be a nightmare.” I don’t think he was convinced that we needed to go to hospital, but he knew by my tone that either he took me or I would take her on my own.

When we arrived at Joondalup Hospital emergency we hadn’t even got to the reception desk and Holly started vomiting again. They took us straight through to a private room and the doctor came and checked her immediately. I told him what had happened from when she got picked up from daycare and also mentioned about the gastro at the daycare so he then started treating her for gastro. He said that if she had been vomiting all night and was dehydrated then she probably had a headache, which made sense. We had to syringe 5mls of hydrolyte into her mouth every 10 minutes and record the times and amounts. She was doing so well, and after an hour started to become a little more alert and started talking and pointing out the posters in the room “Happy Feet” on one side of the bed and “Little Mermaid” on the other side. We got through the first 250ml of hydrolyte and everything seemed to be going well.
The nurses said that they also needed to get a urine sample to see if there was a urinary tract infection so they put one of those silver “pie tins” (the ones they make custard tarts in at the bakery) into her nappy to try and catch the wee. “Good luck with that” I was thinking. Imagine having an alfoil tin stuck in your nappy – how uncomfortable.
So we then started on the second cup of hydrolyte and waiting on a wee, which just didn’t want to come. She seemed to be improving all the time so we were feeling relieved so asked the nurse if we could take her home and get her to do a wee and bring the wee back for testing. The nurse said that the doctor didn’t want her to leave until she had done a wee and said that she should have done a wee by now so that was concerning him. I then told Graeme to go home as it wasn’t any point us both being there waiting, and that I would call him when the doctor said we could go home.
In the next hour things changed very quickly. Holly still had not done a wee and she got half way through the next cup of hydrolyte and then started vomiting again. She got very pale suddenly, and while I was watching her I realized her chest was moving in and out very rapidly. I lifted her shirt and could see her chest just heaving up and down. I called the nurse and she came in to check her and she put the heart monitor on. Suddenly all the alarms started going off on the machine and I asked the nurse what was wrong with her chest that it looked like it was about to explode. She said she would call the doctor to come and check her again.
The doctor came back and said that he would organize some blood tests and called the paediatrician who was on the ward to come and check Holly out. The paediatrician came down within a few minutes and after talking with the initial doctor said that she was sending us off to have X-rays on Holly’s chest to rule out a chest infection. I had rung Graeme and he came straight back to the hospital as we were being taken to the X-rays.
By then it was around 12pm and as we were walking along the long corridor from emergency to the main hospital I was walking on one side of the bed talking with the paediatrician and Graeme was walking on the other side of the bed. The paediatrician then asked me “how long has it been since Holly has moved her head?” I looked over at Holly lying in the bed as it was being wheeled along and noticed that her head was turned towards Graeme but every time I talked her eyes would move to look over at me – but she wasn’t moving her head at all.
I said that I had not even noticed so couldn’t tell her. I said that when we were in the emergency room she had been looking at the posters on the wall from one side to the other, so that had only been an hour or so ago. She then told the nurse to take us to X-rays and that she was going to talk to her colleagues and would see us when we got back.
Once at the X-rays the nurse said that we had to take the silver tray out of Holly’s nappy which was still dry. We took the tray out and put her nappy back on and as soon as I lifted her onto my lap I felt her nappy was warm with wee, and a lot of it. She had been holding on all that time, poor little chicken. She also started to cry and appeared to be in pain, but I couldn’t work out where and I just rubbed her back, but when I touched her she cried more. We had the X-rays done and the doctor said that he could not see any sign of infection.
The nurse wheeled us back to the emergency department and when we walked in we were shocked to see 5 other doctors waiting there with the paediatrician. One of the doctors came forward and introduced herself as the Registrar and her name was Bernadetta. She said that they were there to observe Holly and they had a theory of what may be wrong with her. She asked if she could put her hands underneath Holly’s head to move her head around. We agreed and she moved around to the top of the bed, slid her hands gently under Holly’s head and then tried to turn her head and Holly let out a huge scream. This scream was like nothing I had ever heard in my life – it was the most distressing scream a mum could hear from her child.
I just couldn’t bare it and I remember just yelling at them to stop because they were hurting her.
In that moment there was a flurry of activity and I don’t know how I got through that moment, but I was totally aware of everything being said and I knew that in that moment that something was seriously wrong.
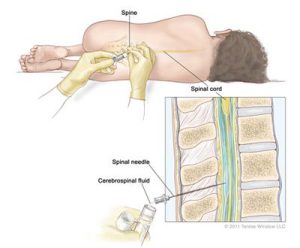
The paediatrician then said to us “we need to do a lumbar puncture.”
I was just devastated but was able to say “yes okay, just do it.”
By then, Graeme was extremely distressed and I told him that he needed to go outside, that I would stay with Holly and that this was what they needed to do to find out what was wrong with her. I surprised myself with how controlled I was and how strong and calm I was. I felt that this was important, it was something that had to be done. I am a big believer in Angels and Spirits and I felt that all that time I was being guided to do what we had to do for Holly. I had absolutely no hesitation in agreeing for them to do the lumbar puncture.
While they were preparing for the lumbar puncture, they then took blood tests and also decided to get Holly’s urine through a catheter. They tried several times to insert the tubing into the urinary tract but it seemed each tube was too thick and because it was taking too long they decided to leave that for the time being and just do the lumbar puncture.
It was around 2pm when they were ready for her. There were two nurses to hold Holly into position. They said that I should wait outside with Graeme, but I refused so they said that I could help to keep her calm by holding her hands and talking to her. In the end, she was so limp and weak that they didn’t need both the nurses to hold her. They rolled her into a foetal position, so one nurse held her in position and I held her hands as she was facing me while I sang nursery rhymes to her.
I remember just before the paediatrician inserted the needle into her spine I asked her “you have done this before, right?”
She looked me right in the eye and she said “Yes I’m the best.”
“Okay” I said “go ahead”.
Holly hardly moved through the whole procedure and just let out a little whimper and a cry as the needle was inserted into her back, and I felt the hot tears falling down my cheeks as her scared eyes looked at me. When it was over one of the nurses said they had never experienced a child so lifeless while having a lumbar puncture before – normally they have to be held into position really tightly.
By this time it was roughly around 2:30pm and I hadn’t had anything to eat apart form a muffin that Graeme had bought me at the café earlier that morning for breakfast. I was starting to feel sick myself and told one of the nurses I felt like I was going to faint. She then asked if I had eaten anything and when I told her I hadn’t she took it on herself to get me a plate of sandwiches and some juice. We suddenly became the focal point of everyone on duty – there were so many people around us there to offer support and help any way they could and I felt very thankful and relieved.
The testing side of things was over probably quicker than what I thought at the time, and by 3pm we were taken through to an isolated room on the paediatric ward to wait. Holly was hooked up to a drip and by then she was just so weak that she just slept and was totally oblivious to what was going on. They weren’t able to tell us too much and said that they had sent the fluid from the lumbar puncture straight to the Chief Microbiologist at PMH who would contact them when he knew something.

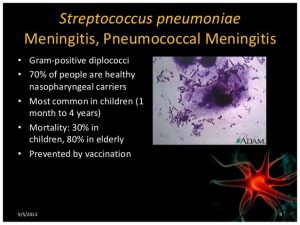
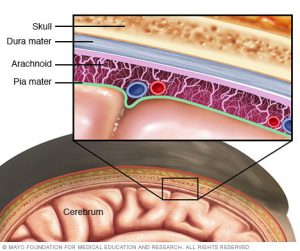
At around 5pm two of the doctors came back and told us that Holly had Pneumococcal Meningitis and that she was a very sick little girl. They said that the fluid in her spine had been very cloudy where normally it would be clear so they knew that the bacteria had spread all the way day the spinal cord and this was not a good sign.
They explained that the microbiologist was growing the bacteria and then would treat each culture with antibiotics to find out which one would kill it. In the meantime they were going to give her 4 different types of antibiotics along with an anti-inflammatory and pain killers through an IV to get her through until they knew.
They told us that this was a critical time and that we needed to prepare ourselves for the worst as she was a very sick little girl. She was too sick to move to Princess Margaret Hospital so they were liaising with the microbiologist and specialists but they assured us that we had the best team possible working with Holly.
She had swelling and inflammation on the brain so they said they would continue to give her 4 high doses of steroids per day to help. The paediatrician told us that normal inflammation levels are around 10 but Holly’s was at 157 on that first night and then jumped up to 340 the following day.
It was just heartbreaking seeing her in so much pain when she moved and they were giving her as much pain killers as they could. She couldn’t lie on her back or be lifted as that pulled on the nerves along the spinal cord and meninges which made her scream and she couldn’t wear any clothing or have the blanket on as that also caused her pain. It was obvious that she had the pain in her spine when we first went to Xrays and that was why when I was stroking her she was in pain as her sensitivity had increased.
We were very well looked after by all the nursing staff and specialists and her two paediatricians spent a lot of time with us and Holly. One of them told us to imagine ourselves with our worst ever hangover and then multiply that by 10 and that is the kind of headache that Holly would be experiencing.
The microbiologist then contacted our hospital team to instruct them to use penicillin for Holly.
For 5 days we just watched her lifeless, unresponsive body lying in bed, hooked up to all sorts of machines and drips praying for our rainbow baby to get better after a gut-wrenching morning of Holly screaming in pain (which saw me really break down in a blubbering mess for the first time after having to hold it all together for so long).
It wasn’t until day 6 that things really improved in the afternoon quite suddenly and then continued to do so.
She became a little bit more responsive and the doctor then came to tell us that her inflammation counter had come down to 19 (the normal level is 10) so they now knew that she had turned the corner. The doctor said it was still a long road ahead with treatment but she had taken a good step forward on the road to recovery.
On Day 8 I was just bursting with happiness as Holly was wide awake, was eating, giggling and we could see the sparks shining in her beautiful blue eyes. She was so good that her doctor said that we could take her in the wheelchair for a walk. We got her in the chair hooked up with all her tubes and machinery but then the nurse said “you won’t be able to go outside as its wet and rainy out there” and with that the clouds parted, the sun shone brightly through the window, the rain stopped and there was a massive rainbow outside the window – it was incredible!
The Universe was letting us know that it was time for Holly to get some fresh air.

By day 9 Holly had improved remarkably. She was sitting up, eating, talking, laughing and being a cheeky monkey and even giving us some attitude but we loved every minute of it. The doctor said that we would still be in hospital for at least another 7 days as she still needed the penicillin through the IV to ensure that they killed off every bit of the bacteria. Her painkillers were reduced and she seemed so much more comfortable. She couldn’t stand or walk unassisted, but she had started pulling herself up by herself on the bed to a sitting position so that was a really good sign.
The doctors were really pleased with her progress but said that the microbiologist had said that because of the severity of her condition there were no short cuts – that we were stuck there until they were sure that the bacteria had been fully treated.
By Day 11 the doctors said that the next few days would be more about getting her mobile as she was still not able to walk unassisted (although we had seen an improvement), but the doctor was confident that she just needed to get her strength back in her legs so we were doing push ups with her legs – (her pushing her feet against our hands) to try and strengthen the muscles.
It wasn’t until day 12 that we learned the full extent of Holly’s illness. Graeme had a lengthy talk with the paediatrician as we wanted to know and understand some of the treatment and procedures still being done and she then told him that Holly had also developed Septicaemia (blood poisoning from the infection) and her inflammation count had risen over 420, but they had decided not to tell us that at the time.
No wonder she was so sick, no wonder we were being prepared for the worst and no wonder she had been in so much pain that no one especially someone so little should have to endure. Bless her to have come through this and still be smiling.
She is definitely a fighter and our little miracle in so many ways.

On day 15 the specialist paediatrician came and gave us the good news that Holly’s blood tests and cultures had come back all clear and told us that Holly was being released the next day and I started to cry – big, happy sobs of joy.
He gave me a hug and then asked what had prompted us to bring her to hospital so quickly. I told him that I felt it in my gut that something was really wrong, I felt an urgency to get her to hospital and felt confident in agreeing to do the lumbar puncture. He said that if it hadn’t been for us getting her to the hospital when we did that it would have been a completely different scenario as the rate the bacteria had developed and grown in a short period of time indicated that if we had left it another few hours she would either have experienced serious brain damage or would have died.
He congratulated us on realising the seriousness of her condition and getting her to hospital so quickly particularly when she didn’t have the usual symptoms of a rash associated with meningitis.
The next day Holly had her final treatment of penicillin at 6am and we were released at 1pm to go home.

What a perfect end to our terrible ordeal as we drove home we were guided and protected by yet another rainbow and as we pulled into the driveway of our home, there shone another rainbow right over the top of our house.
Holly continued to have tests at Princess Margaret Hospital and has been cleared of any side effects such as hearing loss or brain damage, which we are very thankful for.
Graeme still says that he is thankful that I followed my instincts to take her to hospital when we did.
My advice to all mums is “go with your gut instincts.”
It is better to have a “false alarm” than to suffer the consequences if you were to leave your child for a few hours. At the time I knew something was seriously wrong and every time I tried to brush it off, it just got stronger.
REMEMBER – EVERY SECOND COUNTS!
Now….go and hug your children and feel blessed that they are safe and well.
Please check out Meningitis Centre Australia website http://meningitis.com.au/ for more information about all strains of meningitis, the signs and symptoms and to order a fridge magnet with helpful information and instructions. You will notice Holly’s photo in the banner on their page.
Here is a short video for you to watch called “Two Lives – Two Different Outcomes” which shows how “every second counts”….
CLICK HERE TO WATCH THE VIDEO “TWO LIVES – TWO DIFFERENT OUTCOMES”